Will A New High-Water Mark of Opioid Deaths Mark a Turning
Point?
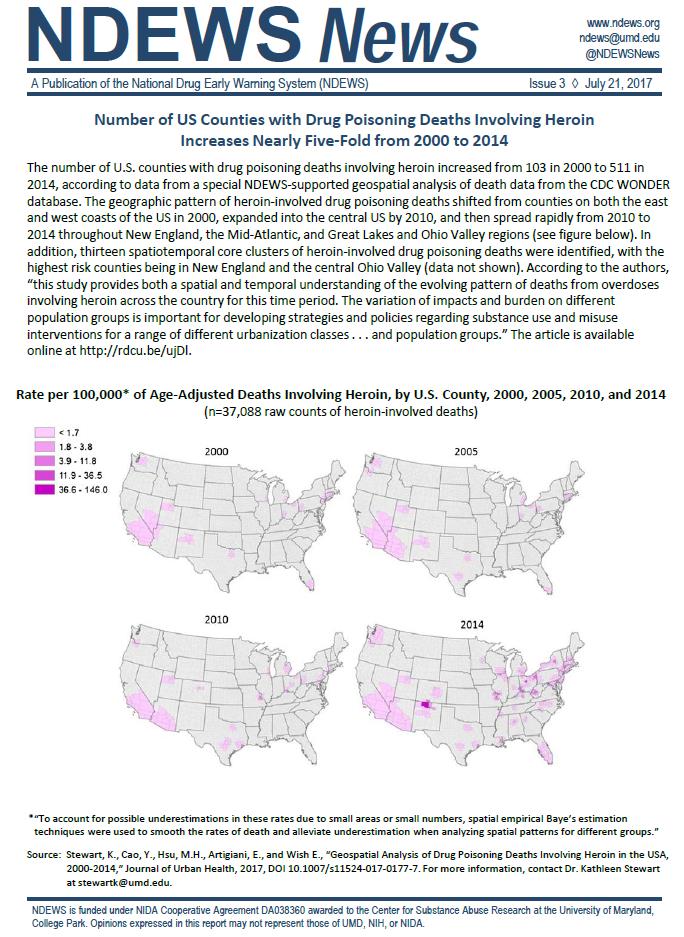
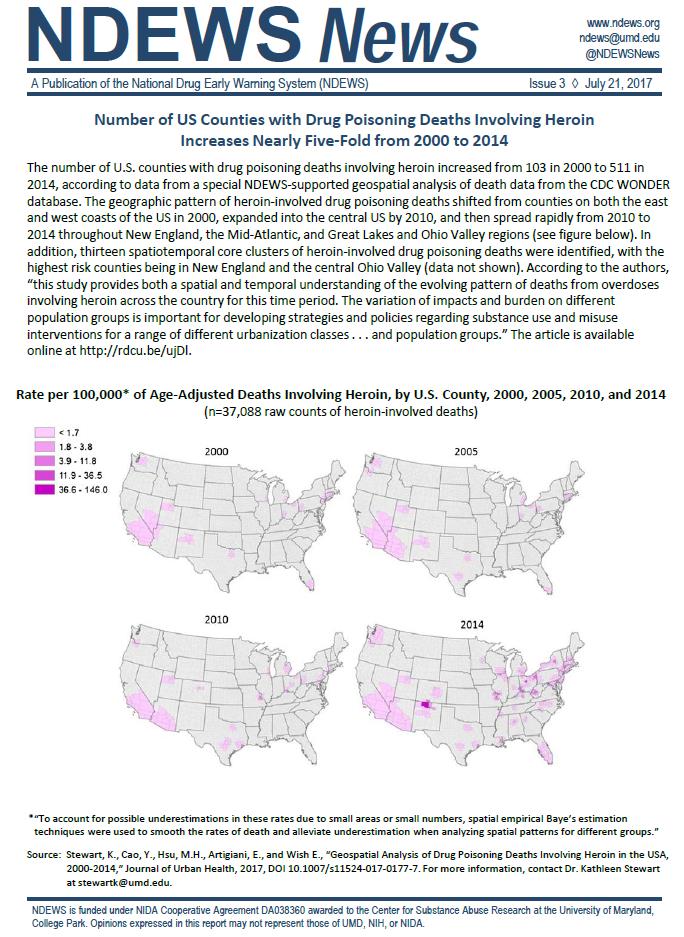
By Rob Chambers
November 23, 2021
The latest provisional data from the Centers for Disease
Control (CDC) shows the U.S. on track to exceed 100,000 overdose deaths in
2021, the first time such a grim milestone would be reached. America clearly
has a drug problem that will require a massive effort from all walks of society
to bring under control.
As one physician put it, the current drug crisis the United
States is experiencing is “worse than the crack epidemic” that upended American
society and brought innumerable amounts of crime and despair to American
cities. But what once was being driven by crack, is now being driven by illicit
opioids, and fentanyl in particular.
A synthetic opioid 50 times more potent than heroin,
fentanyl has increasingly made its way not only into the supply of illicit
opioids but into other drugs such as cocaine and methamphetamines as well. It
is also often pressed into counterfeit prescription pills. All of this has made
drugs even more dangerous than they were in the past. Because even the tiniest
amount can be lethal (2 milligrams, or about 4 grains of salt), users are now
unknowingly ingesting fentanyl with deadly consequences.
Customs and Border Patrol Public Affairs Officer Matthew
Dyman attributes the fentanyl surge in part, to the massive increases in illegal
immigration at the border. The drug is often created in Chinese or Mexican
laboratories and then smuggled across the border by cartels under the cover of
these large migrant caravans. Turning off this fentanyl pipeline will be
critical but breaking the cycle of addiction by expanding access to treatment
programs will also be important.
To date one of the biggest impediments to getting those
suffering from addiction the treatment that they need has been funding, but
that may all be about to change. A landmark settlement recently reached between
a manufacturer and several distributors of prescription opioids and 44 states
across the country promises to provide much needed funding to combat the opioid
crisis. Spearheaded by Texas Attorney General Ken Paxton, as well as several
other Attorneys General across the country, the settlement will provide up to
$26 billion in resources at one of the lowest points of the opioid crisis.
Part of this settlement should go towards supporting
faith-based treatment programs, which have a track record of success. Federal
funds have already been cleared for such purposes – the Department of Health
and Human Services previously affirmed that states may use opioid response
grant funds to support substance use disorder treatment by faith-based
organizations – so it makes sense that private dollars flowing to states from
this settlement should follow suit. Furthermore, given the fact that the Biden
Administration appears to have recognized the value of the faith community by reestablishing
the White House Office of Faith-Based and Neighborhood Partnerships, I hope
that the Federal government will continue to uphold this guidance as well.
As these funds expand access to medication assisted
treatment programs, we must also ensure that patients are treated with the
right medications. The Biden Administration has previously waivered on
expanding access to one of the most commonly used medications to treat opioid
addiction, buprenorphine. After reversing a Trump Administration plan in
February of this year that would have eased rules that unnecessarily limited
physicians’ ability to prescribe the drug, President Biden again reversed
himself in April and reinstated the rule.
While an encouraging change in policy, such uncertainty
could open the door for alternative treatments such as using marijuana to treat
opiate use disorder. Trading one drug for another is not a solution for
addiction and neither federal policy or dollars nor funds from this settlement should
go towards such treatments.
It is often said that it is darkest just before the dawn.
Hopefully we have reached a high-water mark for drug overdose related deaths
that will soon mark a turning point in the opioid crisis. Immediate access to
additional funds for addiction treatment programs will be an encouraging start,
and this will hopefully be part of the movement that will mark the beginning of
a broader trend of society turning away from drugs.
Rob Chambers is the President of the American Council on
Addiction and Alcohol Problems.
FDA Approves Higher Dosage of Naloxone Nasal Spray to Treat Opioid Overdose
For Immediate Release:
April 30, 2021
The U.S. Food and Drug Administration announced today the approval of a higher dose naloxone hydrochloride nasal spray product to treat opioid overdose. The newly approved product delivers 8 milligrams (mg) of naloxone into the nasal cavity. The FDA had previously approved 2 mg and 4 mg naloxone nasal spray products.
Naloxone is a medicine that can be administered by individuals with or without medical training to help reduce opioid overdose deaths. If naloxone is administered quickly, it can counter the opioid overdose effects, usually within minutes. A higher dose of naloxone provides an additional option in the treatment of opioid overdoses.
“Today’s action meets another critical need in combatting opioid overdose,” said Patrizia Cavazzoni, M.D., director of the FDA’s Center for Drug Evaluation and Research. “Addressing the opioid crisis is a top priority for the FDA, and we will continue our efforts to increase access to naloxone and place this important medicine in the hands of those who need it most.”
COVID-19: Online and Remote Resources for Addiction Support
Partnership to End Addiction offers various support options during this difficult time.
Click here to find addiction support for families and individuals.
Are There Any Alternatives When A Physician Offers My Child Opioids for Pain?
Originally Published July 18, 2018
BY COREY W. HUNTER, MD, FIPP
Drugfree.org
Whether your child has struggled with opioid dependence or other substance use issues previously, or whether you’re just concerned about the current opioid crisis, there’s good reason to want your child’s pain to be managed – if possible – by something other than prescription opioid pills. Eventually, your child might have an orthopedic injury or need a tooth pulled at the dentist, so what happens then?
While opioid medications may be effective for treating pain in the short-term, they have an extremely high propensity for addiction and do nothing to address the underlying cause of the pain.
The good news is that there are many alternatives to opioids that can help alleviate your child’s pain.
All Hands on Deck Needed to End the Opioid Crisis
The United States is currently fighting one of the worst addiction problems in its history by way of the opioid crisis. While many Americans are aware of its existence, few likely understand the ongoing issues surrounding this large-scale public health emergency and the extent to which it is undermining the foundations of our great country.
The human and financial toll of this crisis is staggering. In 2018 alone over
47,000 people died from opioid-related overdoses. Meanwhile, a recent analysis from the
Society of Actuaries found that over a four-year period from 2015 to 2018, the total economic cost of the opioid crisis was $631 billion.
This crisis is also destroying families and stretching social service programs to the brink. During that same four-year period, an additional $39 billion was spent on child and family assistance programs and education programs. Every day children are separated from their drug-addicted parents who can no longer care for them and are entered into the foster care system. Babies are born with opiate dependencies, forcing them to confront the scourge of addiction right from the start of their lives. The financial costs certainly can’t be overlooked but it is these intangible societal costs of the opioid crisis that might be the greatest concern of all.
This is why it is so important policymakers in Washington work to identify and counter the drivers of today’s opioid crisis. Increased public education, updated prescribing protocols, and a series of legislative and regulatory efforts aimed at shutting down bad actors have helped significantly reduce the amount of excess prescription pain medication in the country. As a result, the nature of the crisis has morphed from a prescription problem into a heroin crisis and now a full-blown fentanyl epidemic.
It is not hard to see why overdose deaths have spiked significantly since the widespread adoption of fentanyl. A synthetic opioid 50 to 100 times more potent than heroin, just 2 milligrams – the equivalent of 4 grains of salt – is enough to cause a fatal overdose. Curbing the supply of this drug will be key to kicking our country’s current opioid addiction.
The largest suppliers of illicit fentanyl are Chinese laboratories and Mexican drug cartels. The two often work in concert to deliver this deadly drug to our streets.
The majority of fentanyl and its precursors are manufactured in Chinese laboratories and shipped to Mexico. From there, the drug works its way into the drug supply many ways before it is smuggled over the border by the drug cartels.
A common activity is to press fentanyl into counterfeit prescription pills, called “Mexican oxy.” Other times the cartels lace heroin products with the synthetic opioid to provide users with a greater high and to pad their profit margins. And other times the drug is smuggled in its raw form into the United States where it is processed and distributed by affiliate gangs within our borders.
The sheer volume of fentanyl entering the country demonstrates how pressing of an issue this has become. In 2018 alone, almost
1,800 pounds of fentanyl was confiscated at the border, a more than 2500% increase since 2015. That is just what was caught—never mind what made it through.
Fortunately, Congress is considering a number of measures to help curb the supply of this drug. Several versions of a bill called the Fentanyl Sanctions Act are currently under consideration. This legislation would not only direct the president to identify foreign traffickers of opioids on an annual basis, it would also provide law enforcement and sanctions targeteers with a number of precision economic and financial tools to cripple their operations.
To truly end this addiction crisis, we must be sure to also take action to help curb the demand for these drugs as well. As Surgeon General Jerome Adams has pointed out, the country could do well to leverage “
the special talents and calling of the faith community” when combatting the opioid crisis. The Department of Health and Human Services has already affirmed that states may use opioid response grant funds to support substance use disorder treatment services by faith-based organizations. Policymakers at the state and local level should take advantage of these special resources and Washington should continue to support these efforts wherever possible.
Ending the opioid crisis once and for all is an all-hands-on-deck endeavor. A collaborative effort from law enforcement, elected officials, and members of civil society will be required to end these senseless overdose deaths and ensure a healthy drug-free America.
Healthy Pregnancy Healthy Baby Fact Sheets
SAMHSA www.samhsa.gov
This series of four fact sheets emphasizes the importance of continuing a mother's treatment for opioid use disorder (OUD) throughout pregnancy. The series includes information on OUD and pregnancy, OUD treatment, neonatal abstinence syndrome, and considerations to address before hospital discharge.
How Teenage Vaping Puts Structure in Place for Heroin and Cocaine Addiction
THE RAPID ADOPTION OF E-CIGARETTES HAS BEEN DRIVEN, AT LEAST IN PART, BY A HUGE JUMP IN THE POTENCY OF E-LIQUIDS.
By Indra Cidambi, M.D.
June 13, 2018
U.S. News & World Report
CIGARETTE SMOKING AMONG teenagers is on the wane. While data show smoking among teenagers has dropped over the past few years, it's not all good news. Teenagers are vaping nicotine instead. One in 8 – or 12 percent of – teenagers in New Jersey have tried e-cigarettes and/or hookah at least once. When cigarette smoking and nicotine vaping are added together, nicotine use may actually have increased. The rapid adoption of e-cigarettes has been driven, at least in part, by the huge jump in the potency of e-liquids (both nicotine and marijuana) used in vapes. Nicotine and marijuana act on the brain in ways similar to other substances of abuse and prime the brain for addiction to other potent drugs down the road.
Exponential Jump in E-Liquid Potency
Part of the reason for the adoption of e-cigarettes by teenagers is the exponential jump in the potency of e-liquids (nicotine and marijuana) used in vapes. E-liquid products like JUUL contain nearly 50 milligrams of nicotine per milliliter of liquid, whereas a cigarette has about 12 milligrams of nicotine. THC content in liquid concentrates, used in vapes, can range between 50 and 90 percent, as compared to 20 percent in marijuana. Vaping high-concentration marijuana can deliver a more intense high, but it can also lead to addiction.
Get Opioid Resources and Personal Support Sent Straight to Your Phone Via Text
APRIL 16, 2018 BY THE PARTNERSHIP
Help + Hope by Text - SMS messages about opioids
The opioid epidemic in our country has impacted countless families. Unfortunately, the needs of parents and caregivers are often neglected by mainstream care, and every day more families are turning to us for help and support.
We’d like to introduce you to Help & Hope by Text, a way to get customized, mobile messages on your cell phone that provide you with personalized, ongoing support and relevant resources for families struggling with heroin and other opioids.
In other words, parents and caregivers who are concerned with their son’s or daughter’s opioid use can sign up to receive text messages —informed by parents who have been there themselves — containing evidence-based resources, tips, skills, support and hope. Parents can also text “CHAT” to connect with one of our Parent Helpline Specialists at any time, if and when they’re ready.
Click here to visit the Partnership for Drug Free Kids website for opioid resources and personal support.
Introducing the Heroin, Fentanyl & Other Opioids eBook
Partnership for Drug Free Kids
Fueled by drugs like heroin, fentanyl and the misuse of prescription pain pills, the opioid epidemic in our country has impacted countless families.
If your son or daughter is actively using opioids, you’re probably experiencing many negative emotions and concerns. You’re not alone in this struggle. We hope that the information and resources in this guide will empower you with the important tools and guidance you need to help you, your child and your family.
Featured News: Naloxone Administration May Lead to Complications
Partnership for Drug Free Kids www.drugfree.org
FEBRUARY 8, 2018 BY CELIA VIMONT
There seem to be a growing number of cases of high amounts of fluid in the lungs – known as noncardiogenic pulmonary edema – following administration of the opioid overdose antidote naloxone, experts said at a recent meeting of the New York Society of Addiction Medicine annual meeting.
“The cause of naloxone-associated pulmonary edema is unclear. It may be that it is part of the natural history of opioid overdose, and we are just seeing it more often because we have the ability to save patients using an antidote. It could also be because when we wake people with naloxone, they try to take a deep breath against a closed airway, causing barotraumas – injuries caused by increased air or water pressure,” says Nicholas Nacca, MD, Assistant Professor of Emergency Medicine and Medical Toxicologist at the University of Rochester Medical Center.
There is no hard data to support that this phenomenon has increased in frequency, but it certainly seems to be the case, he said. “The dose and route of administration have changed recently. Naloxone is now available in 4-milligram intranasal doses, which is higher than what we have used in the past,” said Dr. Nacca. “Previously, naloxone was available in 2-milligram doses.” In the controlled setting of an emergency room, toxicologists recommend giving the lowest dose of naloxone possible to reverse the respiratory arrest. This is different than in the field, where first responders, police and lay persons are using preloaded intranasal drug delivery devices. “Lives are being saved by these doses of naloxone, and at this time, complications may be a necessary evil,” he said.
Illicit Fentanyl Use Linked to Cases of Amnesia
FEBRUARY 1, 2018 BY PARTNERSHIP NEWS SERVICE STAFF
More than a dozen people who used fentanyl, either alone or in combination with stimulants, have suffered severe memory loss, researchers from West Virginia University report.
These cases involved severe short-term memory loss, HealthDay reports. Imaging scans revealed the patients had lesions on the hippocampus, a region of the brain associated with memory. The patients did not recovery quickly, and may never fully regain their short-term memory, according to lead researcher Marc Haut.
“They all have difficulty learning new information, and it’s pretty dense,” Haut said. “Every day is pretty much a new day for them, and sometimes within a day they can’t maintain information they’ve learned.” He added, “Based upon the imaging, I would be surprised if they didn’t have at least some significant memory problems permanently.”
The findings are published in the Annals of Internal Medicine.
Click here to read the article with clickable links.
A Tide of Opioid-Dependent Newborns Forces Doctors to Rethink Treatment
By CATHERINE SAINT LOUIS
JULY 13, 2017
https://www.nytimes.com/
RICHMOND, Ky. — Just 24 hours old, Jay’la Cy’anne Clay already was having a rough day.
Convulsions rocked her tiny body as she lay under warming lights in the nursery of the Baptist Health Richmond hospital. She vomited and made strange, high-pitched cries.
The infant was going through opioid withdrawal.
For more than a decade, her mother, Jamie Clay, 28, had been hooked on oxycodone. For six months now, she had been in a recovery program, taking another opioid that eased her addiction but put her baby at risk for withdrawal.
From 2003 to 2012, the last year for which statistics are available, the number of babies born dependent on drugs grew nearly fivefold in the United States. Opioids are the main culprit, and states like Kentucky are particularly hard-hit: 15 of every 1,000 infants here are born dependent on opioids.
Babies with the worst withdrawal symptoms are routinely separated from their mothers and whisked by ambulance, at great expense, to hospitals hours away, filling up beds intended for newborns who have even more serious problems, like heart defects.
Urban medical centers nationwide are scrambling to expand neonatal intensive care units or to build separate facilities to accommodate a tide of opioid-exposed babies arriving from rural communities.
The result, many experts say, is an exercise in good intentions gone awry.
This isn’t the first U.S. opiate-addiction crisis
By Stephen Mihm
The U.S. is in the throes of an “unprecedented opioid epidemic,” the Centers for Disease Control and Prevention reports. The crisis has spurred calls for action to halt the rising death toll, which has devastated many rural communities.
It’s true that there’s an opioid epidemic, a public health disaster. It’s not true that it’s unprecedented. A remarkably similar epidemic beset the U.S. some 150 years ago. The story of that earlier catastrophe offers some sobering lessons as to how to address the problem.
Scout project teaches Erie-area parents signs of addiction
By Madeleine O’Neill
https://www.goerie.com
Jul 17, 2017
COREY EISERT-WLODARCZYK BUILT THE INTERIOR OF A MOBILE TRAILER DESIGNED TO LOOK LIKE A TEENAGER’S BEDROOM AND TEACH SIGNS OF DRUG ABUSE.
To parents, picking up on the signs of drug addiction in their teenager’s bedroom might seem daunting.
Corey Eisert-Wlodarczyk wants to help change that.
“I think that the front line dealing with youth in the heroin and opioid crisis is the parents,” said Eisert-Wlodarczyk, 17.
For his Eagle Scout project, Eisert-Wlodarczyk built and decorated the interior of a Hidden in Plain Sight mobile display that looks like a teenager’s bedroom and can be used to show parents common indicators of drug abuse.
Eisert-Wlodarczyk knows the tragic costs of the heroin crisis: he lost his older brother, Collin Eisert-Wlodarczyk, to an accidental heroin overdose in 2012.
“A big part of that for me is just having the ability to use my loss to change the community to benefit others,” he said.
His work on the trailer is aimed at providing as many parents as possible with tools to recognize warning signs of drug addiction, which could be as subtle as a piece of foil or a water bottle with a false bottom. Eisert-Wlodarczyk is a member of Boy Scout Troop 52 in Millcreek Township and is entering his senior year at McDowell High School.
The Public Cost Of Heroin: $51,000 A Year Per User, UIC Study Says
By DNAinfo Staff | June 13, 2017
www.dnainfo.com
THE LOOP — Heroin users in the United States cost society about $51,000 per year in terms of treatment, infectious disease, prison and lost productivity, a team at the University of Illinois Chicago has determined.
UIC pharmacoeconomists led by Simon Pickard and Ruixuan Jiang estimated that 1 million people in the United States are "active heroin users," costing the country $51 billion per year.
Meet Chef Jesse Schenker: An All-Star Chef in Recovery
Partnership for Drug Free Kids
www.drugfree.org
APRIL 21, 2017 BY JULIE
We recently met up with Chef Jesse Schenker, executive chef and owner of The Gander and author of All or Nothing: One Chef’s Appetite for the Extreme. We’re thrilled that Schenker will be the VIP chef at our All-Star Tasting event on May 31, 2017 in New York City and are grateful for his honesty in sharing his recovery story with us.
PARTNERSHIP FOR DRUG-FREE KIDS: Could you first give us a little background on yourself, both personally and professionally?
CHEF JESSE SCHENKER: Growing up in South Florida, I experienced epicurean pleasures that quickly ignited my passion and set me on the path toward becoming a chef. I began requesting menus from my parents’ dinners and invested in a cookbook collection that has since grown to nearly 350 volumes.
I channeled my excitement for food into a Culinary Degree at the Atlantic Technical Center in Coconut Creek, Florida. While in school, I was introduced to my first professional kitchen experience at Café Maxx under the tutelage of Chef Oliver Saucy. I then moved on to hold positions in the kitchens of some of Florida’s most celebrated restaurant like Chef Mark Militello’s James Beard award-winning restaurant Mark’s on Las Olas and City Cellar Wine Bar & Grill. I then moved to New York to refine my skills in some of the world’s finest restaurants. I accepted a position as Chef de Partie as the two-Michelin star rated Gordon Ramsay at the London where I stayed for a year and a half.
I opened my first restaurant Recette, an intimate, urban American restaurant in New York’s West Village, in January of 2010. Just months after its opening, Recette received glowing two-star reviews from both The New York Times and New York Magazine.
In 2014, I wrote my memoir, All or Nothing: One Chef’s Appetite for the Extreme to reflect on my journey from growing up as an anxious child in a tight-knit family to a homeless teenager with a heroin addiction by the time I was 19 years old — and the journey back.
PARTNERSHIP: Tell us about your recovery story. What helps to maintain your recovery today?
SCHENKER: I first smoked pot when I was about 11. I knew something inside of me was forever changed. It wasn’t typical experimentation; I became different. I became me without the anxiety. The marijuana use escalated over my teenage years. I used acid, took painkillers, pretty much whatever I could get my hands on. The straw that broke the camel’s back for me was OxyContin. I quickly became hooked to this powerful opioid and when I couldn’t get my hands on any, I did whatever any person with a burgeoning addiction did in the 90’s: I switched to heroin and developed a full-blown heroin addiction by the time I was 18.
Things had to get very, very bad for me to get to a place where I was ready to begin recovery. I had been through rehab/detox a number of times. Didn’t matter. My parents gave me a choice: drugs or family. I chose drugs. From that point on, I was on my own until I was arrested. I served six months in jail and then another six months in a drug rehab facility for inmates. Following that was six months in a work release/halfway house. The moment I was arrested was the moment I decided to turn my life around.
I was ready — I was cold, alone, homeless and unemployed. I was determined to rebuild my life. Jail saved my life. I was very ill initially from the withdrawal of heroin, it was extremely painful. Once the physical withdrawal passed, I had intense drug dreams and flashbacks. I immersed myself in the 12-step program, and everyone said, “Keep coming back.” Well, I did, and I still attend AA/ NA meetings to this day. I learned to take what I need, and leave the rest. I learned that as long as I stayed clean and sober, I could rebuild my life.
And I did. I went from track marks and jail stints to a fulfilling life as a New York City chef with my wonderful wife and two kids, Eddie who is 6 and Liv who is 2.
PARTNERSHIP: Why are you excited to be working with us?
SCHENKER: Because I’m passionate about ensuring that people have the resources and the community around them to deal with this issue head-on. I want to see the shame eliminated from the families and individuals who struggle with drug addiction. Kids (and their parents) aren’t the sum total of the bad choices that they have made. We need competent mental health counselors who understand the complex issues of addiction today.
I remember being in a clinic when I was on methadone and someone asking me how a nice Jewish kid from a nice family ended up this way. Drugs don’t discriminate. It doesn’t matter how much socio-economic wealth you had or didn’t have. It doesn’t matter if you are Christian, Jewish or Muslim. It doesn’t matter if you attended an Ivy League university. We are all vulnerable to the effects of drug addiction.
PARTNERSHIP: How does your recovery impact your approach to parenting?
SCHENKER: I am very honest with my kids, in the most age appropriate way that I can be. Drugs and alcohol will be a part of our conversation once it’s more appropriate. I think it’s up to us to really educate our kids about the dangers, and the pitfalls, and also what it means to have an addiction. There’s definitely a biological component, so just as you would want to know if your parents have high blood pressure, it’s important that they understand that I struggled with addiction.
There’s also this overwhelming desire that parents have today to make their kids happy. This is not the paradigm by which my wife and I parent. Happiness, something so fickle and so different for each individual, must be cultivated from within. Our children will have to figure that part out on their own for themselves. What we can do, is to teach them how to lead moral and productive lives. That is what we strive for one day at a time.
PARTNERSHIP: Do you have any advice for parent with a child who is struggling with drugs or alcohol?
SCHENKER: I get asked this question quite often. The truth is that every family is different. I think the best thing a parent can do is have their eyes wide open. Denial is powerful. I remember something my parents told me: You can only blame yourself and feel guilty for so long. When I was out on the street, they decided to get into Al-Anon and work on themselves, so that when I came around, they too would be healthy. They had to learn all over again how to set healthy boundaries for themselves and what it means to be a parent. What they needed to provide and what they didn’t. Thank God they did, it saved my life.
PARTNERSHIP: What do you like to cook with/for your kids?
SCHENKER: We are a big barbeque family. Every Sunday we cook on an open outdoor grill. My son will collect the firewood from our yard. We will roast potatoes, fresh leeks, onions and whatever meat or fish looks most appealing that day: sausage, langoustines, octopus, a whole pig — you name it, we’ve done it.
The best thing as a parent is to watch your kids eat really good, nourishing food. I’ll throw together a salad with arugula, cashews, fresh ricotta cheese, mint and I’ll dress it with lemon juice and olive oil. My kids will actually eat it — it’s a win-win.